Urinary Tract Infections (UTIs) are common bacterial infections that affect the urinary system. They can manifest in various forms, with cystitis and pyelonephritis being two distinct types of UTIs. While both conditions involve bacterial invasion of the urinary tract, they differ in terms of their symptoms, diagnosis, treatments, and prognosis. This essay aims to compare and contrast cystitis and pyelonephritis along these dimensions to provide a comprehensive understanding of these prevalent medical conditions. Included are a summary table and multiple choice practice questions and answers. Enjoy!

Symptoms of Cystitis
Cystitis, often referred to as a lower UTI, primarily affects the bladder and urethra. It is typically characterized by a distinct set of symptoms:
- Frequent Urination: One of the hallmark symptoms of cystitis is the frequent urge to urinate. Patients may find themselves rushing to the bathroom more often than usual.
- Dysuria: Dysuria, or a burning sensation during urination, is another common symptom. This discomfort is often a source of distress for individuals with cystitis.
- Hematuria: Hematuria, the presence of blood in the urine, can occur in cystitis. It may cause the urine to appear pink or reddish.
- Cloudy or Foul-Smelling Urine: The urine in cystitis cases may become cloudy and have an unpleasant odor.
- Lower Abdominal Discomfort: Some individuals with cystitis may experience mild to moderate lower abdominal discomfort or pressure.
- Urinary Urgency: Patients often feel a strong and urgent need to urinate, even if their bladder is not full.
Symptoms of Pyelonephritis
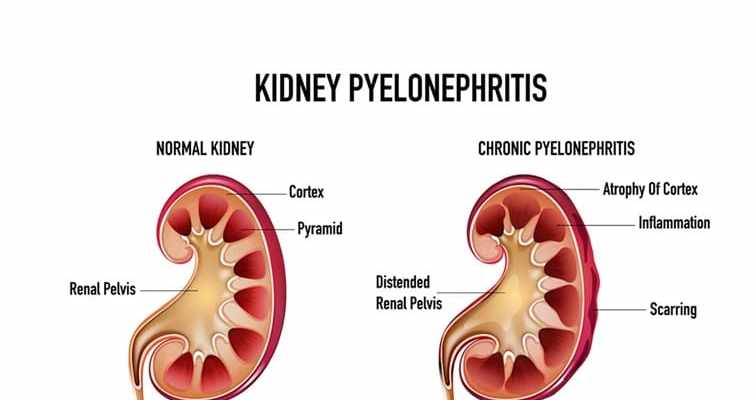
Pyelonephritis, classified as an upper UTI, affects the kidneys and is associated with more severe symptoms that can be systemic in nature:
- High Fever: Pyelonephritis commonly causes a high fever, often accompanied by chills. The fever is typically higher than what is seen in cystitis cases.
- Flank or Back Pain: Pyelonephritis is characterized by intense pain in the flank or back region, typically on one side. This pain can be severe and radiate towards the lower abdomen.
- Nausea and Vomiting: Individuals with pyelonephritis may experience nausea and vomiting, which can lead to dehydration if not adequately managed.
- General Malaise: Patients with pyelonephritis often report feeling unwell, fatigued, and generally sick.
- Urinary Symptoms: In addition to the systemic symptoms, pyelonephritis can exhibit the same urinary symptoms as cystitis, such as dysuria, frequency, and urgency.
- Potentially Severe Complications: If left untreated, pyelonephritis can lead to serious complications, including kidney abscesses or scarring, which can cause long-term kidney damage.
In comparing cystitis and pyelonephritis in terms of symptoms, several key differences emerge. Cystitis primarily affects the lower urinary tract and is characterized by localized symptoms such as frequent urination, dysuria, and hematuria. It rarely leads to systemic illness. In contrast, pyelonephritis involves the kidneys and is associated with more severe and systemic symptoms, including high fever, intense back pain, nausea, vomiting, and a general sense of unwellness.
Additionally, while both types of UTIs can cause urinary urgency and dysuria, pyelonephritis symptoms tend to be more severe and are often accompanied by a high fever, making it easier to differentiate from cystitis.
Diagnosing Cystitis
Diagnosing cystitis, a lower UTI primarily affecting the bladder, typically involves the following steps:
- Medical History and Physical Examination: The healthcare provider will start by taking a detailed medical history, asking about symptoms, previous UTIs, and any risk factors. A physical examination may also be conducted to assess for signs of discomfort or tenderness in the lower abdomen.
- Urinalysis: A urinalysis is a crucial diagnostic tool for cystitis. It involves analyzing a urine sample to look for signs of infection, such as the presence of white blood cells, red blood cells, bacteria, and abnormal pH levels. A positive urinalysis suggests a possible UTI.
- Urine Culture: In some cases, especially if the infection is recurrent or complicated, a urine culture may be performed. This test identifies the specific bacteria causing the infection and helps determine the most effective antibiotic treatment.
- Imaging: Imaging studies such as ultrasound or CT scans are typically not required for diagnosing uncomplicated cystitis. However, if there are recurrent episodes or other concerning factors, these imaging techniques may be used to assess for structural abnormalities.
Diagnosing Pyelonephritis
Pyelonephritis, an upper UTI affecting the kidneys, requires a more comprehensive diagnostic approach due to its potential for serious complications. The diagnostic process for pyelonephritis involves:
- Medical History and Physical Examination: Similar to cystitis, the healthcare provider will begin with a thorough medical history and physical examination, paying particular attention to symptoms like fever, back pain, and systemic signs of infection.
- Urinalysis and Blood Tests: A urinalysis is a crucial initial step in diagnosing pyelonephritis. It will show elevated white blood cells, bacteria, and may reveal hematuria. Blood tests, including a complete blood count (CBC) and comprehensive metabolic panel (CMP), are used to assess kidney function and to detect markers of inflammation or infection, such as elevated white blood cell counts and C-reactive protein (CRP) levels.
- Urine Culture: Similar to cystitis, a urine culture may be performed to identify the specific bacteria responsible for the infection and determine antibiotic sensitivity. This helps tailor antibiotic therapy effectively.
- Imaging: Imaging studies play a more significant role in the diagnosis of pyelonephritis. A renal ultrasound is often used as an initial imaging tool to assess the kidneys for signs of inflammation, swelling, or abscesses. In more complex or severe cases, a contrast-enhanced CT scan may be necessary to provide detailed information about kidney function and anatomy.
The diagnostic process for cystitis and pyelonephritis shares some common elements, including a medical history, physical examination, urinalysis, and urine culture. However, the diagnosis of pyelonephritis involves additional steps, such as blood tests and imaging studies, to evaluate kidney function and identify potential complications. The presence of systemic symptoms, such as high fever and intense back pain, in pyelonephritis necessitates a more thorough assessment.
CT Abdomen Pelvis showing Acute Pyelonephritis of the Right Kidney

Treatment of Cystitis
Cystitis, a lower UTI that primarily affects the bladder, is generally less severe than pyelonephritis. Treatment for cystitis typically includes:
- Antibiotics: The mainstay of cystitis treatment is oral antibiotics. Commonly prescribed antibiotics for uncomplicated cases include trimethoprim-sulfamethoxazole (TMP-SMX), nitrofurantoin, and fosfomycin. These antibiotics are usually taken for a short course, often ranging from 3 to 7 days.
- Increased Fluid Intake: Patients with cystitis are advised to drink plenty of fluids, primarily water. This helps flush out bacteria from the urinary tract and alleviate symptoms.
- Pain Management: Over-the-counter pain relievers, such as ibuprofen or acetaminophen, may be recommended to manage any discomfort or pain associated with cystitis.
- Avoiding Irritants: Patients are often advised to avoid irritants like caffeine, alcohol, and spicy foods, which can exacerbate bladder irritation.
- Evaluation for Complications: In some cases, if cystitis recurs frequently or is associated with other concerning factors, further evaluation may be needed to identify any underlying issues, such as urinary tract abnormalities.
Treatment of Pyelonephritis
Pyelonephritis, an upper UTI affecting the kidneys, is typically more severe than cystitis and may require more aggressive treatment. The treatment for pyelonephritis includes:
- Hospitalization: Many cases of pyelonephritis require hospitalization, especially if the patient is experiencing high fever, severe pain, vomiting, or dehydration. Hospitalization allows for close monitoring and intravenous (IV) administration of antibiotics.
- Intravenous Antibiotics: IV antibiotics, such as ceftriaxone or ciprofloxacin, are often administered to ensure rapid and effective treatment of pyelonephritis. Hospitalization allows for continuous administration and close monitoring of antibiotic therapy.
- Adequate Hydration: Patients with pyelonephritis are at risk of dehydration due to fever and vomiting. Intravenous fluids are often administered to maintain hydration and support kidney function.
- Pain Management: Severe back pain and discomfort associated with pyelonephritis may require stronger pain medications, such as opioids, for adequate relief.
- Addressing Underlying Causes: In cases where pyelonephritis is recurrent or associated with anatomical or functional issues in the urinary tract, surgical intervention may be necessary to prevent further episodes.
The treatment of cystitis and pyelonephritis differs significantly based on the severity and location of the infection. Cystitis is generally treated with oral antibiotics on an outpatient basis and is often self-limiting. The emphasis is on symptom relief and eliminating the infection from the bladder.
In contrast, pyelonephritis requires hospitalization and intravenous antibiotics due to its potential for severe complications, including kidney damage and sepsis. The goal is to treat the infection rapidly, manage systemic symptoms, and prevent long-term kidney impairment.

Prognosis of Cystitis
Cystitis, often referred to as a lower UTI, primarily affects the bladder and is characterized by localized symptoms. The prognosis for cystitis is generally favorable, with several key points to consider:
- Resolution: With appropriate treatment, cystitis typically resolves within a few days to a week. Oral antibiotics like trimethoprim-sulfamethoxazole (TMP-SMX), nitrofurantoin, or fosfomycin are effective in eradicating the infection.
- Minimal Long-Term Consequences: In uncomplicated cases of cystitis, there are typically no long-term consequences or complications. Once the infection clears, patients return to their normal urinary function without ongoing issues.
- Recurrence: Some individuals may experience recurrent episodes of cystitis, which can be bothersome but are generally not associated with severe long-term health effects. Recurrence may prompt further evaluation to identify underlying causes.
- Prevention: Preventive measures, such as staying well-hydrated, urinating regularly, and proper hygiene, can help reduce the risk of future cystitis episodes.
Prognosis of Pyelonephritis
Pyelonephritis, classified as an upper UTI, affects the kidneys and can lead to more significant health implications. The prognosis for pyelonephritis varies depending on several factors:
- Prompt Treatment: Early diagnosis and prompt treatment of pyelonephritis are critical for a favorable prognosis. Hospitalization is often required to administer intravenous antibiotics and manage symptoms effectively.
- Resolution and Kidney Function: With appropriate treatment, most cases of acute pyelonephritis resolve completely, and kidney function returns to normal. This is especially true for uncomplicated cases.
- Risk of Complications: If left untreated or inadequately managed, pyelonephritis can lead to complications such as kidney abscesses, scarring, or the development of chronic kidney disease (CKD). Recurrent episodes of pyelonephritis may increase the risk of these complications.
- Long-Term Monitoring: In some cases, especially when complications occur, patients may require long-term monitoring of kidney function and ongoing medical management to prevent recurrence and mitigate complications.
In comparing the prognosis of cystitis and pyelonephritis, it becomes evident that cystitis generally has a more favorable outlook. Cystitis is typically a self-limiting condition with minimal long-term consequences when adequately treated. Recurrent episodes can be bothersome but are not typically associated with severe health issues.
On the other hand, pyelonephritis, especially if left untreated or if complications arise, has the potential for more significant long-term consequences. While most cases of acute pyelonephritis resolve completely with prompt and appropriate treatment, there is a risk of kidney damage and chronic kidney disease in severe or recurrent cases.
In conclusion, cystitis and pyelonephritis are two distinct types of UTIs with varying prognoses. Cystitis is generally associated with a favorable prognosis, with most cases resolving completely and minimal long-term consequences. In contrast, pyelonephritis, particularly in severe or recurrent cases, can lead to kidney damage and chronic kidney disease. Early diagnosis, prompt treatment, and long-term monitoring are crucial factors in determining the prognosis of these UTIs. Healthcare providers must consider the specific type of UTI and individual patient factors when assessing and managing these infections to ensure the best possible outcomes.
Summary Table:
Urinary Tract Infections (UTI) – Cystitis vs Pyelonephritis: Symptoms, Diagnosis, Treatments, and Prognosis
Here’s a summary table comparing and contrasting Urinary Tract Infections (UTI) – Cystitis vs. Pyelonephritis in terms of Symptoms, Diagnosis, Treatments, and Prognosis:
| Aspect | Cystitis | Pyelonephritis |
|---|---|---|
| Symptoms | – Frequent urination | – High fever |
| – Dysuria (burning during urination) | – Severe back/flank pain | |
| – Hematuria (blood in urine) | – Nausea and vomiting | |
| – Cloudy or foul-smelling urine | – General malaise | |
| – Lower abdominal discomfort | – Urinary symptoms (dysuria, urgency) | |
| – Urinary urgency | ||
| Diagnosis | – Urinalysis | – Urinalysis |
| – Urine culture | – Blood tests (CBC, CRP) | |
| – Physical examination | – Imaging (ultrasound, CT) | |
| – Imaging (if necessary) | – Urine culture | |
| – Physical examination | ||
| Treatments | – Oral antibiotics | – Hospitalization (in severe cases) |
| – Increased fluid intake | – Intravenous antibiotics | |
| – Pain management (if needed) | – Adequate hydration | |
| – Avoiding irritants | – Pain management (stronger medications) | |
| – Evaluation for complications | – Addressing underlying causes | |
| Prognosis | – Favorable, minimal long-term consequences | – Favorable with prompt treatment |
| – Recurrence possible | – Risk of complications (e.g., kidney damage) | |
| – Minimal long-term consequences | – Potential for chronic kidney disease (CKD) | |
| – Proactive prevention measures | – Long-term monitoring (in severe cases) |
Multiple Choice Practice Questions and Answers
Multiple-Choice Questions
- What is a common symptom of both cystitis and pyelonephritis?A) High fever B) Cloudy urine C) Lower abdominal discomfort D) Severe back pain
- Which type of UTI primarily affects the bladder?A) Cystitis B) Pyelonephritis C) Urethritis D) Prostatitis
- What is the mainstay of treatment for cystitis?A) Intravenous antibiotics B) Increased fluid intake C) Surgery D) Avoiding caffeine
- Which diagnostic test is common for both cystitis and pyelonephritis?A) CT scan B) Blood culture C) Physical examination D) Urinalysis
- What is a distinguishing symptom of pyelonephritis compared to cystitis?A) Frequent urination B) Cloudy urine C) Severe back pain D) Dysuria
- In which type of UTI is hospitalization often required?A) Cystitis B) Urethritis C) Pyelonephritis D) Prostatitis
- What is the main objective of treatment in pyelonephritis?A) Pain management B) Reducing urinary urgency C) Intravenous fluids D) Intravenous antibiotics
- What can recurrent episodes of cystitis prompt healthcare providers to do?A) Prescribe stronger antibiotics B) Recommend preventive measures C) Perform a blood culture D) Conduct further evaluation
- What is the long-term consequence most commonly associated with untreated or recurrent pyelonephritis?A) Urinary urgency B) Kidney damage C) Cloudy urine D) Lower abdominal discomfort
- What is a recommended preventive measure for both cystitis and pyelonephritis?A) Avoiding spicy foods B) Drinking cranberry juice C) Increasing caffeine intake D) Staying well-hydrated
Answer Explanations
- Answer: B) Cloudy urine
- Explanation: Both cystitis and pyelonephritis can result in cloudy urine due to the presence of white blood cells, bacteria, and other elements associated with infection.
- Answer: A) Cystitis
- Explanation: Cystitis primarily affects the bladder, leading to symptoms such as frequent urination and lower abdominal discomfort.
- Answer: B) Increased fluid intake
- Explanation: While antibiotics are used to treat cystitis, increasing fluid intake (usually water) is an important part of the management to help flush out bacteria.
- Answer: D) Urinalysis
- Explanation: Both cystitis and pyelonephritis are typically diagnosed with urinalysis to detect signs of infection, such as white blood cells and bacteria.
- Answer: C) Severe back pain
- Explanation: Severe back pain or flank pain is a characteristic symptom of pyelonephritis and is not typically associated with cystitis.
- Answer: C) Pyelonephritis
- Explanation: Hospitalization is often necessary for severe cases of pyelonephritis, especially when patients exhibit high fever, severe pain, and dehydration.
- Answer: D) Intravenous antibiotics
- Explanation: Prompt administration of intravenous antibiotics is crucial to effectively treat pyelonephritis and prevent complications.
- Answer: D) Conduct further evaluation
- Explanation: Recurrent episodes of cystitis may prompt healthcare providers to conduct further evaluation to identify underlying causes or contributing factors.
- Answer: B) Kidney damage
- Explanation: Untreated or recurrent pyelonephritis can lead to kidney damage, including scarring or abscess formation.
- Answer: D) Staying well-hydrated
- Explanation: Adequate hydration is a preventive measure for both cystitis and pyelonephritis, as it helps flush out bacteria from the urinary tract and maintain urinary health.
Check out these popular articles 🙂
Circulatory System: Blood Flow Pathway Through the Heart
Ectoderm vs Endoderm vs Mesoderm
Circulatory System: Heart Structures and Functions
Ductus Arteriosus Vs Ductus Venosus Vs Foramen Ovale: Fetal Heart Circulation
Cardiac Arrhythmias: Definition, Types, Symptoms, and Prevention
Upper Vs Lower Respiratory System: Upper vs Lower Respiratory Tract Infections
Seven General Functions of the Respiratory System
Digestive System Anatomy: Diagram, Organs, Structures, and Functions
Kidney Embryology & Development: Easy Lesson
Psychology 101: Crowd Psychology and The Theory of Gustave Le Bon
Introduction to Evolution: Charles Darwin and Alfred Russel Wallace
Copyright © 2024 Moosmosis Organization: All Rights Reserved
All rights reserved. This essay first published on moosmosis.org or any portion thereof may not be reproduced or used in any manner whatsoever
without the express written permission of the publisher at moosmosis.org.

Please Like and Subscribe to our Email List at moosmosis.org, Facebook, Twitter, Youtube to support our open-access youth education initiatives! 🙂
Categories: anatomy, Biology, cell biology, education, health, medicine, stem, technology








Thank you for this detailed research it is very interesting.
LikeLiked by 1 person
Thank you so much Charlotte!! Have a good day!
LikeLike