Crohn’s disease and ulcerative colitis (UC) affect millions and are both types of inflammatory bowel disease (IBD) that affect the gastrointestinal tract. This essay aims to compare and contrast Crohn’s Disease and Ulcerative Colitis, shedding light on their clinical presentations, underlying mechanisms, diagnostic approaches, treatment options, and prognosis. Included are a summary table and multiple choice practice questions and answers. Enjoy!
Symptoms:
Similar Symptoms in Crohn’s Disease and Ulcerative Colitis:
- Diarrhea: Both conditions often present with diarrhea, which may be frequent and urgent. In both cases, diarrhea can be accompanied by mucus or blood.
- Abdominal Pain: Abdominal pain and cramping are common in both Crohn’s disease and UC. The location and severity of pain can vary depending on the specific location of inflammation.
- Fatigue: Chronic inflammation and the body’s response to it can lead to fatigue in both conditions.
- Weight Loss: Unintended weight loss can occur in both Crohn’s disease and UC due to reduced nutrient absorption and loss of appetite.
Differences in Symptoms:
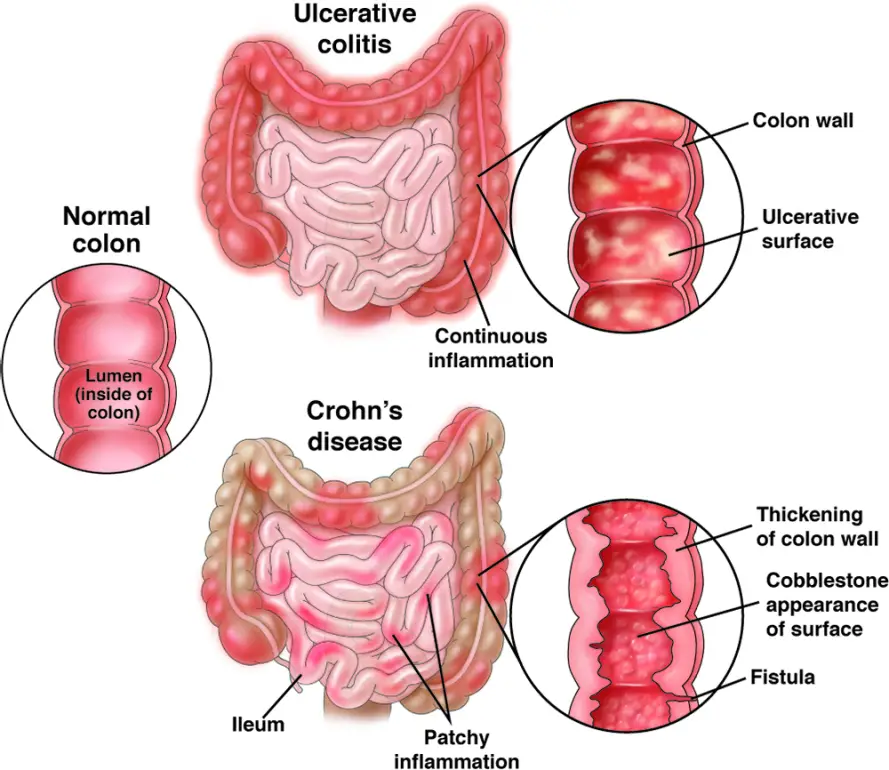
- Location of Inflammation:
- Crohn’s Disease: It can affect any part of the digestive tract from the mouth to the anus. Therefore, symptoms can occur in various areas, including the small intestine, colon, and other parts of the GI tract. This variability can lead to a wide range of symptoms.
- Ulcerative Colitis: UC primarily affects the colon (large intestine) and rectum. Symptoms are typically limited to the lower part of the digestive tract.
- Rectal Bleeding:
- Crohn’s Disease: While it can cause gastrointestinal bleeding, rectal bleeding is less common in Crohn’s compared to UC.
- Ulcerative Colitis: Rectal bleeding is a hallmark symptom of UC and often presents as blood in the stool.
- Types of Pain:
- Crohn’s Disease: Pain can be more intermittent and “crampy,” and it may not always correlate directly with bowel movements. It can also be experienced in multiple areas of the abdomen.
- Ulcerative Colitis: Pain is often continuous and more localized to the lower abdomen, especially around the rectum.
- Extraintestinal Symptoms:
- Crohn’s Disease: Crohn’s can affect other parts of the body, leading to symptoms such as joint pain, skin rashes, and eye inflammation.
- Ulcerative Colitis: UC primarily affects the colon, so it is less likely to cause extraintestinal symptoms.
- Pattern of Inflammation:
- Crohn’s Disease: Characterized by “skip lesions,” meaning there are inflamed areas of the intestine alternating with healthy sections.
- Ulcerative Colitis: Inflammation tends to be continuous, typically starting in the rectum and extending upward into the colon.
Diagnosis:
Common Diagnostic Methods for Crohn’s Disease and Ulcerative Colitis:
- Medical History and Physical Examination: The process usually begins with a detailed medical history where the healthcare provider asks about symptoms, their duration, and any relevant family history. A physical examination may also be conducted to check for signs such as abdominal tenderness or mass.
- Blood Tests: Blood tests can be used to assess inflammation markers (e.g., C-reactive protein and erythrocyte sedimentation rate) and check for anemia or nutritional deficiencies. These markers can be elevated in both Crohn’s disease and UC.
- Endoscopy: Both conditions often require endoscopic procedures to visualize the inside of the gastrointestinal tract. These procedures include:
- Colonoscopy: Used to examine the entire colon and rectum. Biopsies can be taken during colonoscopy to confirm the diagnosis and assess the extent of inflammation.
- Sigmoidoscopy: Similar to colonoscopy but examines only the lower part of the colon and rectum.
- Biopsies: During endoscopy, tissue samples (biopsies) may be taken from the affected areas for microscopic examination. Biopsies can help differentiate between Crohn’s disease and UC and determine the severity of inflammation.
Differences in Diagnosis:
- Imaging Studies:
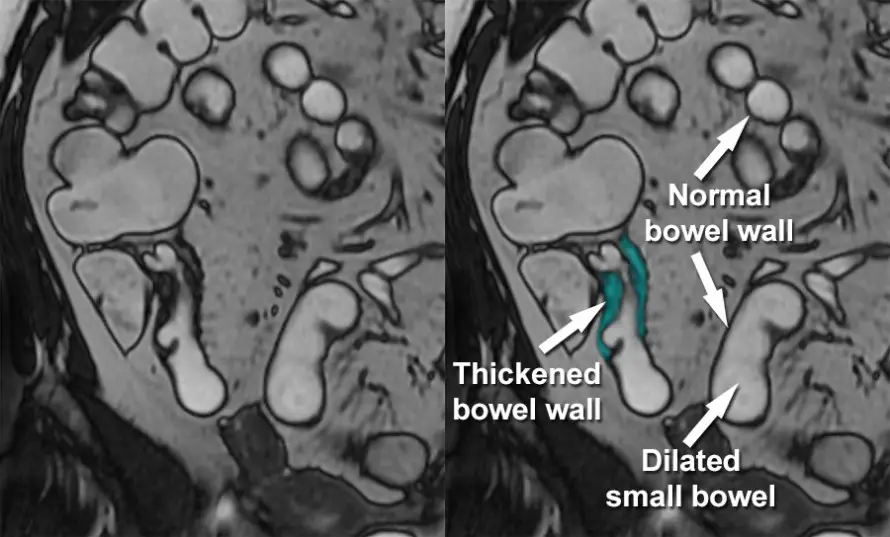
- Crohn’s Disease: Additional imaging studies like CT scans, MRIs, or capsule endoscopy may be necessary to evaluate the entire gastrointestinal tract as Crohn’s disease can affect any part of it. Imaging can also help identify complications such as strictures and fistulas.
- Ulcerative Colitis: UC primarily affects the colon and rectum, so imaging studies beyond the lower digestive tract are usually not needed for diagnosis.
- Pattern of Inflammation:
- Crohn’s Disease: Characterized by “skip lesions,” meaning there are inflamed areas of the intestine alternating with healthy sections. This pattern can be observed through imaging and endoscopy.
- Ulcerative Colitis: Inflammation tends to be continuous, typically starting in the rectum and extending upward into the colon. This pattern is evident during colonoscopy and sigmoidoscopy.
- Diagnostic Criteria:
- Crohn’s Disease: Diagnosis often relies on the presence of characteristic features such as transmural inflammation and skip lesions. It may also involve ruling out other conditions with similar symptoms.
- Ulcerative Colitis: Diagnosis is based on the presence of continuous inflammation in the colon and rectum. If the inflammation extends beyond the rectum, it is classified as UC.
MRI showing Crohn’s Disease with Thickening of the Bowel in a Skip Lesion
Treatments:
Similar Treatment Approaches:
- Medications: Both Crohn’s disease and UC are often initially managed with medications to control inflammation and symptoms. Common medications include:
- Aminosalicylates (5-ASAs): Used to reduce inflammation in mild to moderate cases and are more commonly associated with UC.
- Corticosteroids: Prescribed for short-term relief of acute symptoms and to induce remission.
- Immunomodulators: Such as azathioprine or 6-mercaptopurine, used to suppress the immune system and maintain remission.
- Biologics: These newer medications, like infliximab or adalimumab, target specific immune pathways and are often used for moderate to severe cases or when other treatments fail.
- Nutritional Support: Nutritional therapy may be used in both conditions, particularly during flare-ups. Enteral nutrition (liquid formulas) or total parenteral nutrition (TPN) can provide essential nutrients and give the digestive system a rest.
- Lifestyle Modifications: Lifestyle changes, including dietary modifications, stress management, and regular exercise, can help manage symptoms and improve overall health for individuals with both Crohn’s disease and UC.
Differences in Treatment:
- Surgery:
- Crohn’s Disease: Surgical intervention is more common in Crohn’s disease due to complications like strictures, fistulas, and abscesses. Surgery may involve the removal of diseased sections of the intestine, but the disease can recur in other areas.
- Ulcerative Colitis: Surgery can provide a potential cure for UC in severe cases. Total colectomy (removal of the colon) with or without ileal pouch-anal anastomosis (IPAA) can eliminate symptoms and the risk of colorectal cancer.
- Medication Choices:
- Crohn’s Disease: The choice of medication often depends on the location and severity of inflammation. Biologics are frequently used in moderate to severe cases and when other treatments fail.
- Ulcerative Colitis: Aminosalicylates are commonly used as first-line treatment in UC. Biologics are also used for moderate to severe cases, but UC tends to respond more favorably to aminosalicylates.
- Pattern of Inflammation:
- Crohn’s Disease: Treatment may need to address complications like strictures or abscesses. Medications and surgery may be targeted at specific areas of inflammation.
- Ulcerative Colitis: Treatment typically focuses on the extent of inflammation within the colon and rectum.
- Extraintestinal Symptoms:
- Crohn’s Disease: Treatment may involve addressing extraintestinal symptoms such as joint pain, skin issues, or eye inflammation.
- Ulcerative Colitis: UC primarily affects the colon, so extraintestinal manifestations are less common.
Prognosis:
Crohn’s Disease Prognosis:
- Chronic Nature: Crohn’s disease is a chronic condition characterized by periods of active disease (flare-ups) and remission. It often has a more unpredictable course compared to UC.
- Complications: Crohn’s disease can lead to various complications such as strictures, fistulas, abscesses, and the formation of intestinal obstructions. These complications may require surgical intervention.
- Recurrence: Even after surgical removal of the affected portion of the intestine, Crohn’s disease can recur in other parts of the digestive tract. Recurrence is common and needs ongoing management.
- Extraintestinal Manifestations: Crohn’s disease can affect other parts of the body, leading to extraintestinal symptoms such as joint pain, skin rashes, and eye inflammation. Managing these symptoms may require additional medical care.
- Cancer Risk: There is a slightly increased risk of colorectal cancer in individuals with Crohn’s disease, especially in long-standing and extensive cases. Regular surveillance and monitoring are important.
Ulcerative Colitis Prognosis:
- Colon-Specific: UC primarily affects the colon and rectum. Unlike Crohn’s disease, it typically does not involve other parts of the digestive tract or extraintestinal organs.
- Potential for Cure: In some severe cases of UC, surgical removal of the entire colon (total colectomy) can provide a potential cure. This procedure eliminates symptoms and the risk of colorectal cancer.
- Remission: UC often responds well to treatment, and many individuals can achieve long-term remission with the appropriate medications. Symptom management becomes a key focus.
- Limited Complications: While UC can lead to complications such as severe bleeding, toxic megacolon, or the development of pouch-related issues after surgery, the overall risk of complications may be somewhat lower than that of Crohn’s disease.
- Cancer Risk: There is an increased risk of colorectal cancer in individuals with UC, particularly those with long-standing and extensive disease. Regular surveillance and monitoring through colonoscopy are crucial for early detection.
In summary, the prognosis for Crohn’s disease and ulcerative colitis differs in terms of the chronicity, location of symptoms, potential for cure, and complications. Crohn’s disease is more likely to involve complications, extraintestinal symptoms, and recurrent disease in different parts of the gastrointestinal tract. In contrast, UC is more colon-specific, with a potential cure through surgery in severe cases, and it often responds well to medications for symptom management. Regular monitoring for colorectal cancer risk is important in both conditions. It’s essential for individuals with IBD to work closely with healthcare providers to develop a personalized treatment and monitoring plan that addresses their specific needs and circumstances.
nts experiencing biliary system complications.
Summary Table: Crohn’s Diseases vs Ulcerative Colitis – Symptoms, Causes, Treatments, and Prognosis
| Aspect | Crohn’s Disease | Ulcerative Colitis |
|---|---|---|
| Symptoms | – Abdominal pain – Diarrhea (may be bloody) – Weight loss – Fatigue – Fever – Extraintestinal symptoms (e.g., joint pain, skin rashes) | – Bloody diarrhea – Abdominal pain – Urgency to have a bowel movement – Rectal bleeding – Milder extraintestinal symptoms |
| Diagnosis | – Endoscopy (colonoscopy or sigmoidoscopy) with biopsies – Blood tests (inflammation markers, anemia) – Imaging (CT, MRI) for extent assessment | – Endoscopy (colonoscopy or sigmoidoscopy) with biopsies – Blood tests (inflammation markers, anemia) |
| Treatments | – Medications (aminosalicylates, corticosteroids, immunomodulators, biologics) – Nutritional support – Lifestyle modifications – Surgery (for complications or disease management) | – Medications (aminosalicylates, corticosteroids, immunomodulators, biologics) – Nutritional support – Lifestyle modifications – Surgery (total colectomy for potential cure) |
| Prognosis | – Chronic, with unpredictable flare-ups – Risk of complications (strictures, fistulas, abscesses) – Risk of recurrence after surgery – Extraintestinal manifestations – Slightly increased risk of colorectal cancer | – Chronic but often manageable – Potential for cure through surgery (total colectomy) – Typically fewer complications – Lower risk of extraintestinal manifestations – Increased risk of colorectal cancer, especially with long-standing disease |
Multiple Choice Practice Questions and Answers
1. What is a common symptom shared by both Crohn’s disease and ulcerative colitis?
- A) Joint pain
- B) Chest pain
- C) Headache
- D) Back pain
Answer: A) Joint pain
Explanation: Joint pain, also known as arthralgia, is an extraintestinal symptom that can occur in both Crohn’s disease and ulcerative colitis.
2. Which imaging technique is more likely to be used to assess Crohn’s disease involving the small intestine?
- A) Colonoscopy
- B) Sigmoidoscopy
- C) CT scan
- D) Blood test
Answer: C) CT scan
Explanation: CT scans are often used to evaluate the entire gastrointestinal tract, including the small intestine, in cases of Crohn’s disease.
3. Which of the following is more commonly associated with ulcerative colitis than Crohn’s disease?
- A) Abdominal pain
- B) Weight loss
- C) Extraintestinal symptoms
- D) Fistulas
Answer: C) Extraintestinal symptoms
Explanation: Ulcerative colitis typically involves fewer extraintestinal symptoms compared to Crohn’s disease.
4. What is a potential surgical option for achieving a cure in severe cases of ulcerative colitis?
- A) Appendectomy
- B) Total colectomy
- C) Cholecystectomy
- D) Nephrectomy
Answer: B) Total colectomy
Explanation: Total colectomy, which involves removing the entire colon, is a surgical option that can potentially cure ulcerative colitis.
5. Which of the following is a common treatment approach for inducing remission in both Crohn’s disease and ulcerative colitis?
- A) Total colectomy
- B) Corticosteroids
- C) Immunomodulators
- D) Antibiotics
Answer: B) Corticosteroids
Explanation: Corticosteroids are often used to induce remission in both Crohn’s disease and ulcerative colitis.
6. In Crohn’s disease, what is the term for inflamed areas of the intestine alternating with healthy sections?
- A) Continuous inflammation
- B) Transmural inflammation
- C) Skip lesions
- D) Remission
Answer: C) Skip lesions
Explanation: Crohn’s disease is characterized by “skip lesions,” where inflamed areas of the intestine alternate with healthy sections.
7. Which condition is more likely to involve complications such as strictures, fistulas, and abscesses?
- A) Crohn’s disease
- B) Ulcerative colitis
- C) Both equally
- D) Neither
Answer: A) Crohn’s disease
Explanation: Complications such as strictures, fistulas, and abscesses are more commonly associated with Crohn’s disease.
8. Which inflammatory bowel disease has a slightly increased risk of colorectal cancer associated with it?
- A) Crohn’s disease
- B) Ulcerative colitis
- C) Neither
- D) Both equally
Answer: B) Ulcerative colitis
Explanation: Ulcerative colitis carries a slightly increased risk of colorectal cancer, particularly in cases of long-standing and extensive disease.
9. Which of the following is a primary treatment goal for ulcerative colitis management?
- A) Achieving extraintestinal symptom relief
- B) Minimizing the risk of Crohn’s disease development
- C) Achieving long-term remission
- D) Preventing joint pain
Answer: C) Achieving long-term remission
Explanation: Achieving long-term remission of symptoms is a primary treatment goal in the management of ulcerative colitis.
10. What is the main difference in the pattern of inflammation between Crohn’s disease and ulcerative colitis?
- A) Crohn’s disease has continuous inflammation.
- B) Ulcerative colitis has skip lesions.
- C) Crohn’s disease affects only the colon.
- D) Ulcerative colitis has transmural inflammation.
Answer: B) Ulcerative colitis has skip lesions.
Explanation: Crohn’s disease is characterized by skip lesions, whereas ulcerative colitis has continuous inflammation, typically starting in the rectum and extending upward into the colon.
Check out these popular articles 🙂
Circulatory System: Blood Flow Pathway Through the Heart
Ectoderm vs Endoderm vs Mesoderm
Circulatory System: Heart Structures and Functions
Ductus Arteriosus Vs Ductus Venosus Vs Foramen Ovale: Fetal Heart Circulation
Cardiac Arrhythmias: Definition, Types, Symptoms, and Prevention
Upper Vs Lower Respiratory System: Upper vs Lower Respiratory Tract Infections
Seven General Functions of the Respiratory System
Digestive System Anatomy: Diagram, Organs, Structures, and Functions
Kidney Embryology & Development: Easy Lesson
Psychology 101: Crowd Psychology and The Theory of Gustave Le Bon
Introduction to Evolution: Charles Darwin and Alfred Russel Wallace
Copyright © 2023 Moosmosis Organization: All Rights Reserved
All rights reserved. This essay first published on moosmosis.org or any portion thereof may not be reproduced or used in any manner whatsoever
without the express written permission of the publisher at moosmosis.org.

Please Like and Subscribe to our Email List at moosmosis.org, Facebook, Twitter, Youtube to support our open-access youth education initiatives! 🙂
Categories: anatomy, Biology, cell biology, education, health, medicine, stem, technology









Very insightful article, well written.
LikeLiked by 2 people
2 very similar and yet different diseases! Helpful thanks
LikeLiked by 2 people
NICE POST 💕💖💓
Blessed and Happy afternoon 🌞
Greetings 👋
I GROW TOGETHER witch feedback 💯 thanks
David López Moncada pk 🌎
LikeLiked by 1 person
Thank you so much!!! 💕💖💓 Have a blessed and happy day!! 🌞
LikeLike