Hello there, my friends! In this lesson, we explore heart attacks and heart failure, which are both important and highly common medical conditions. It is important to differentiate between heart attacks and heart failure as they have different clinical presentations and treatment approaches. Let’s compare and contrast these two types in terms of anatomy, symptoms, diagnosis, treatment, and prognosis.
Heart Attacks and Heart Failure: Anatomy
Heart attack (myocardial infarction) and heart failure are two distinct cardiac conditions that have significant implications for patient health and well-being. While both conditions affect the heart, they differ in their underlying causes, symptoms, pathophysiology, diagnosis, treatment, and prognosis. We aim to provide a comprehensive comparison and contrast of heart attack and heart failure, with a specific focus on the anatomical aspects of these conditions.
Heart Attack Anatomy:
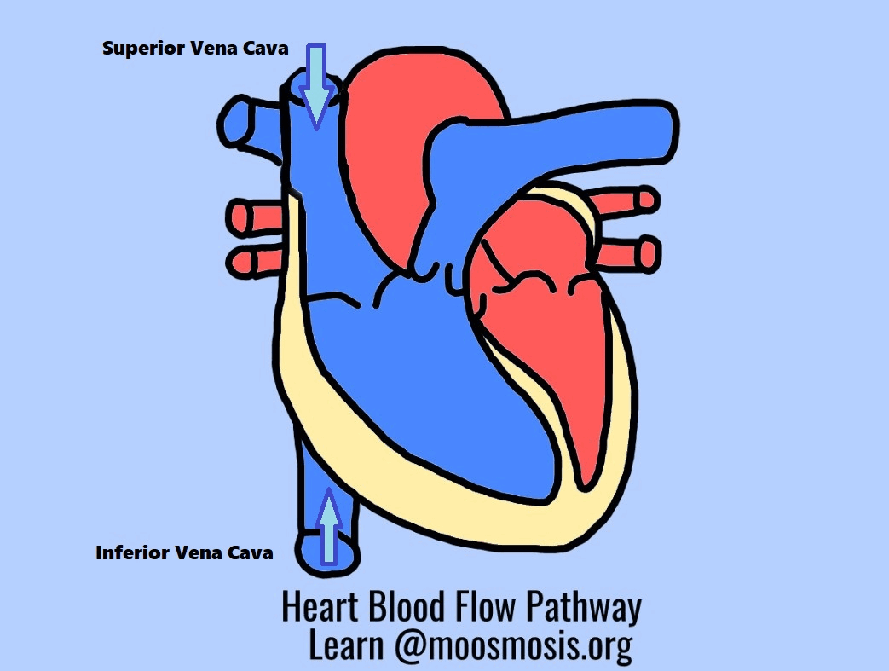
A heart attack occurs when there is a sudden blockage of blood flow to a portion of the heart muscle. The underlying cause is usually the rupture of an atherosclerotic plaque or the formation of a blood clot (thrombus) within a coronary artery. Coronary arteries are responsible for supplying oxygen-rich blood to the heart muscle. When a blockage occurs, the affected area of the heart muscle does not receive adequate blood supply, resulting in ischemia and subsequent tissue damage.
During a heart attack, the blockage usually occurs in one of the coronary arteries, such as the left anterior descending artery, left circumflex artery, or right coronary artery. The specific location of the blockage determines which area of the heart is affected. For example, if the blockage is in the left anterior descending artery, the anterior wall of the left ventricle may be affected.
Heart Failure Anatomy:
Heart failure is a chronic condition characterized by the heart’s inability to effectively pump blood to meet the body’s demands. It can involve the left ventricle, right ventricle, or both. Heart failure can be classified as systolic heart failure, where the heart’s ability to contract and pump blood is impaired, or diastolic heart failure, where the heart’s ability to relax and fill with blood is compromised.
The anatomy involved in heart failure includes the heart chambers, valves, and surrounding structures. When heart failure affects the left ventricle, it can lead to an increased pressure within the left atrium and pulmonary circulation. This can result in the accumulation of fluid in the lungs, causing symptoms such as shortness of breath and coughing. Right-sided heart failure primarily affects the right ventricle and can lead to fluid retention in the body, resulting in swelling of the ankles and legs.
Comparison and Contrast of Anatomy:
While both heart attack and heart failure involve the heart, their anatomical differences are notable. A heart attack is typically caused by a sudden blockage in a coronary artery, leading to ischemia and damage to a specific area of the heart muscle. In contrast, heart failure is characterized by a progressive weakening of the heart’s pumping ability, affecting either the left ventricle, right ventricle, or both. It involves the entire heart and its chambers, valves, and associated structures.
Heart attack primarily affects a specific area of the heart muscle that is supplied by the blocked coronary artery, whereas heart failure can involve the entire heart and its chambers. Heart failure may lead to changes in the structure and function of the heart over time, including chamber dilation, thickening of the heart walls, and valvular abnormalities. In heart failure, the impairment of both the left and right sides of the heart can occur simultaneously or progress gradually from one side to the other.
Conclusion: Heart attack and heart failure differ in their anatomical manifestations within the heart. A heart attack involves a sudden blockage of blood flow to a specific area of the heart muscle, while heart failure encompasses the impaired pumping or filling of the heart chambers, affecting the left ventricle, right ventricle, or both. Understanding the anatomical distinctions between these conditions is vital for accurate diagnosis, appropriate treatment strategies, and improved patient outcomes.
Heart Attacks and Heart Failure: Symptoms
Heart attack (myocardial infarction) and heart failure are two distinct cardiac conditions that can have significant implications for a patient’s health and well-being. While both conditions affect the heart, they differ in their underlying causes, anatomical manifestations, pathophysiology, diagnosis, treatment, and prognosis. We aim to provide a comprehensive comparison and contrast of heart attack and heart failure, focusing specifically on the symptoms associated with each condition.
Symptoms of Heart Attack: A heart attack typically manifests with sudden and intense symptoms that require immediate medical attention. The most common symptom is chest pain or discomfort, often described as a crushing, squeezing, or tight sensation. This pain may radiate to the arms, shoulders, neck, jaw, or back. Other symptoms include:
- Shortness of breath: Difficulty breathing or feeling breathless even at rest or during minimal exertion.
- Nausea and vomiting: Sensation of nausea and sometimes vomiting may occur.
- Lightheadedness: Feeling dizzy or lightheaded, potentially leading to fainting.
- Cold sweats: Profuse sweating that feels cold and clammy.
Symptoms of Heart Failure: Heart failure symptoms can develop gradually and worsen over time as the heart’s pumping ability decreases. The symptoms can vary depending on whether the left or right side of the heart is predominantly affected. Common symptoms of heart failure include:
- Fatigue and weakness: Feeling tired and lacking energy, even with minimal physical activity.
- Shortness of breath: Difficulty breathing, especially during exertion or when lying flat, often accompanied by a persistent cough or wheezing.
- Swelling: Fluid retention resulting in swelling of the ankles, legs, abdomen, or veins in the neck.
- Rapid or irregular heartbeat: Palpitations or a sensation of the heart racing or beating irregularly.
Differences in Symptoms: While there may be some overlapping symptoms between heart attack and heart failure, certain distinctions can help differentiate between the two conditions.
Heart Attack Symptoms:
- Chest pain or discomfort is a hallmark symptom of a heart attack, often described as a crushing or squeezing sensation. This symptom is typically absent in heart failure.
- The intensity of symptoms during a heart attack is usually more abrupt and severe compared to heart failure.
- Nausea, vomiting, and cold sweats are more commonly associated with a heart attack rather than heart failure.

A heart attack is characterized by sudden and intense chest pain or discomfort, along with symptoms such as shortness of breath, nausea, lightheadedness, and cold sweats.
Heart Failure Symptoms:
- Fatigue and weakness are prominent symptoms in heart failure and often present even at rest or with minimal exertion. These symptoms are less characteristic of a heart attack.
- Swelling (edema) in the ankles, legs, or abdomen is more commonly seen in heart failure due to fluid retention. This symptom is typically absent in heart attack.
- Shortness of breath, especially during exertion or when lying flat, is a hallmark symptom of heart failure and can be accompanied by a persistent cough or wheezing. These symptoms are less prominent in a heart attack.
Conclusion: Heart attack and heart failure differ in their symptomatology, which can aid in their differentiation. A heart attack is characterized by sudden and intense chest pain or discomfort, along with symptoms such as shortness of breath, nausea, lightheadedness, and cold sweats. In contrast, heart failure is characterized by fatigue, shortness of breath, swelling, and rapid or irregular heartbeat. Understanding these symptom differences is crucial for prompt diagnosis, appropriate treatment, and improved patient outcomes.

A heart failure is characterized by fatigue, shortness of breath, swelling, and rapid or irregular heartbeat.
Heart Attacks and Heart Failure: Diagnosis
Heart attack (myocardial infarction) and heart failure are distinct cardiac conditions that require accurate diagnosis to initiate appropriate treatment strategies. Although both conditions affect the heart, they differ in their underlying causes, symptoms, anatomical manifestations, pathophysiology, treatment, and prognosis. This essay aims to provide a comprehensive comparison and contrast of heart attack and heart failure, with a specific focus on the diagnostic approaches employed for each condition.
Diagnosis of Heart Attack: The diagnosis of a heart attack involves a combination of clinical evaluation, medical history assessment, and diagnostic tests. The following diagnostic approaches are commonly employed:
- Electrocardiogram (ECG): An ECG measures the electrical activity of the heart and helps identify abnormalities associated with a heart attack. It can show characteristic changes, such as ST-segment elevation or depression, suggesting myocardial ischemia or injury.
- Cardiac Enzymes: Blood tests are performed to measure cardiac enzymes, such as troponin and creatine kinase-MB (CK-MB). Elevated levels of these enzymes indicate myocardial damage and help confirm the diagnosis of a heart attack.
- Coronary Angiography: This invasive procedure involves the injection of a contrast dye into the coronary arteries, followed by X-ray imaging. It helps identify the location and severity of coronary artery blockages or narrowings, providing critical information for further treatment planning.
Diagnosis of Heart Failure: The diagnosis of heart failure requires a comprehensive evaluation, including a thorough medical history, physical examination, and diagnostic tests. The following diagnostic approaches are commonly employed:
- Echocardiography: This non-invasive test uses ultrasound waves to assess the structure and function of the heart. Echocardiography can measure the ejection fraction (EF), which is a crucial parameter to determine systolic heart failure. It also evaluates the presence of valve abnormalities or other structural heart defects.
- Blood Tests: Blood tests, such as brain natriuretic peptide (BNP) or N-terminal pro-BNP (NT-proBNP), are helpful in diagnosing heart failure. Elevated levels of these biomarkers indicate myocardial stress and can aid in the assessment of disease severity.
- Chest X-ray: A chest X-ray can reveal signs of heart failure, such as an enlarged heart, fluid accumulation in the lungs (pulmonary edema), or congestion in the blood vessels of the lungs.
- Stress Test: A stress test involves the evaluation of the heart’s response to exercise or medication-induced stress. It helps assess exercise tolerance, detect any abnormal heart rhythms, or identify signs of inadequate blood flow to the heart muscle.
Comparison and Contrast of Diagnosis: Both heart attack and heart failure require a combination of clinical evaluation and diagnostic tests for accurate diagnosis. However, the diagnostic approaches differ in their focus and objectives.
Heart Attack Diagnosis:
- Diagnosis of a heart attack primarily relies on ECG findings, cardiac enzyme levels, and coronary angiography to identify the presence and location of a blockage in the coronary arteries.
- The emphasis is on confirming acute myocardial infarction and determining the need for immediate reperfusion therapy to restore blood flow to the affected area of the heart.
Diagnosis Tools: Diagnosis of Heart Attack: ECG, coronary angiography, cardiac enzymes
Heart Failure Diagnosis:
- Diagnosis of heart failure involves a comprehensive evaluation of symptoms, medical history, physical examination, and a combination of tests, including echocardiography, blood biomarkers (BNP or NT-proBNP), chest X-ray, and stress tests.
- The objective is to assess cardiac structure and function, determine the underlying cause of heart failure, evaluate disease severity, and guide appropriate treatment strategies.
Chest X-Ray of Patient with Congestive Heart Failure

Diagnosis Tools: Diagnosis of Heart Failure: ECHO, blood tests, chest x-ray, stress test
Conclusion: Heart attack and heart failure differ in their diagnostic approaches, reflecting the distinct nature and pathophysiology of each condition. The diagnosis of a heart attack focuses on identifying acute myocardial infarction and determining the need for urgent reperfusion therapy. In contrast, the diagnosis of heart failure involves a comprehensive evaluation of cardiac structure and function to assess disease severity and guide appropriate treatment strategies. Accurate diagnosis plays a crucial role in initiating timely interventions, optimizing patient outcomes, and improving overall cardiac health.
Heart Attacks and Heart Failure: Treatment
Heart attack (myocardial infarction) and heart failure are two distinct cardiac conditions that require specific treatment strategies to improve patient outcomes and quality of life. Although both conditions affect the heart, they differ in their underlying causes, symptoms, anatomical manifestations, pathophysiology, diagnosis, and prognosis. This essay aims to provide a comprehensive comparison and contrast of heart attack and heart failure, focusing on the treatment approaches employed for each condition.
Treatment of Heart Attack: The treatment of a heart attack aims to restore blood flow to the blocked coronary artery and prevent further damage to the heart muscle. Key treatment approaches include:
- Reperfusion Therapy: Reperfusion therapy involves the restoration of blood flow to the blocked coronary artery. This can be achieved through two main strategies: a. Percutaneous Coronary Intervention (PCI): This procedure involves the insertion of a catheter with a balloon into the blocked artery to inflate and open it. In some cases, a stent may be placed to keep the artery open. b. Thrombolytic Therapy: Thrombolytic drugs can be administered to dissolve the blood clot causing the blockage, although PCI is generally preferred when available.
- Medications: a. Antiplatelet Agents: Medications such as aspirin and P2Y12 inhibitors (e.g., clopidogrel) are prescribed to prevent further blood clot formation. b. Beta-Blockers: These drugs help reduce the workload on the heart and improve its function. c. ACE Inhibitors or ARBs: These medications are prescribed to improve heart function, reduce strain on the heart, and prevent further remodeling of the heart tissue.
Reperfusion therapy, such as PCI Percutaneous Coronary Intervention, for Heart Attacks

Treatment is reperfusion therapy, such as PCI or thrombolytic therapy, and medications for heart attacks.
Treatment of Heart Failure: The treatment of heart failure aims to improve symptoms, slow disease progression, and enhance overall cardiac function. Key treatment approaches include:
- Medications: a. Diuretics: Diuretics help reduce fluid retention and alleviate symptoms of congestion. b. ACE Inhibitors or ARBs: These drugs improve heart function, reduce strain on the heart, and enhance survival rates. c. Beta-Blockers: Beta-blockers can help improve heart function, decrease heart rate, and manage symptoms. d. Aldosterone Antagonists: These medications may be prescribed in certain cases to reduce fluid retention and improve outcomes. e. Digoxin: Digoxin is used in specific cases to improve symptoms and enhance heart function.
- Device Implantation: a. Implantable Cardioverter-Defibrillator (ICD): An ICD is a device that monitors heart rhythm and delivers an electric shock if a life-threatening arrhythmia occurs. b. Cardiac Resynchronization Therapy (CRT): CRT involves the implantation of a device that coordinates the contractions of the heart chambers, improving overall heart function.
- Lifestyle Modifications: a. Dietary Changes: A heart-healthy diet low in sodium and saturated fats is recommended to manage heart failure. b. Exercise: Regular physical activity tailored to the patient’s condition can help improve cardiac function and overall well-being. c. Fluid Restriction: In some cases, limiting fluid intake may be necessary to manage fluid retention.
Treatment is medications, device implantation such as ICD or CRT, and/or lifestyle modification for heart failure.
Comparison and Contrast of Treatment: While both heart attack and heart failure require comprehensive treatment approaches, there are notable differences in their management strategies.
Heart Attack Treatment:
- Reperfusion therapy, such as PCI or thrombolytic therapy, is the primary treatment focus to restore blood flow and prevent further damage to the heart muscle.
- Medications are administered to prevent further clot formation, reduce cardiac workload, and promote healing and recovery.
Heart Failure Treatment:
- Medications play a central role in heart failure treatment, aiming to improve symptoms, slow disease progression, and enhance overall heart function.
- Device implantation, such as ICD or CRT, may be considered in select cases to manage arrhythmias and optimize cardiac performance.
- Lifestyle modifications, including dietary changes, exercise, and fluid restriction, are vital in managing heart failure symptoms and promoting overall cardiovascular health.
Conclusion: Heart attack and heart failure necessitate distinct treatment approaches due to their underlying causes and pathophysiology. The treatment of a heart attack focuses on restoring blood flow to the blocked artery through reperfusion therapy, coupled with medications to prevent further clot formation and promote healing. In contrast, heart failure treatment aims to manage symptoms, slow disease progression, and enhance cardiac function through medications, device implantation, and lifestyle modifications. Tailored treatment strategies can significantly improve patient outcomes and quality of life for individuals affected by these cardiac conditions.
Heart Attacks and Heart Failure: Prognosis
Heart attack (myocardial infarction) and heart failure are two distinct cardiac conditions with significant implications for a patient’s long-term prognosis and overall health. While both conditions affect the heart, they differ in their underlying causes, symptoms, anatomical manifestations, pathophysiology, diagnosis, and treatment. This essay aims to provide a comprehensive comparison and contrast of the prognosis associated with heart attack and heart failure.

Prognosis of Heart Attack: The prognosis of a heart attack can vary depending on various factors, including the extent of myocardial damage, the presence of complications, the promptness of medical intervention, and the patient’s overall health status. Key aspects of the prognosis for a heart attack include:
- Short-term Mortality: A heart attack can result in immediate complications, such as arrhythmias, cardiac arrest, or cardiogenic shock, which can be life-threatening. Prompt medical intervention, including reperfusion therapy, improves the prognosis and reduces the risk of short-term mortality.
- Long-term Mortality: Survivors of a heart attack have an increased risk of future cardiovascular events and mortality compared to the general population. The risk is influenced by factors such as the presence of underlying coronary artery disease, residual cardiac damage, lifestyle factors, and adherence to medical therapy.
- Cardiac Function: The extent of myocardial damage and the location of the affected area can impact cardiac function and subsequent prognosis. Left ventricular dysfunction resulting from a heart attack may lead to the development of heart failure, further affecting long-term prognosis.
Prognosis of Heart Failure: The prognosis of heart failure is influenced by multiple factors, including the underlying cause, severity of symptoms, overall cardiac function, response to treatment, and patient adherence to lifestyle modifications and medications. Key aspects of the prognosis for heart failure include:
- Mortality: Heart failure is associated with increased mortality rates, particularly in cases of advanced or severe heart failure. The prognosis is influenced by factors such as the underlying cause, extent of myocardial damage, comorbidities, and response to treatment.
- Disease Progression: Heart failure is a progressive condition, and its prognosis can be influenced by the rate of disease progression. Appropriate management strategies, including medications, device implantation, and lifestyle modifications, aim to slow disease progression and improve prognosis.
- Quality of Life: Heart failure can significantly impact a patient’s quality of life due to symptoms such as fatigue, breathlessness, and reduced exercise tolerance. Effective management strategies that alleviate symptoms and improve cardiac function can positively impact a patient’s quality of life.
Comparison and Contrast of Prognosis: While both heart attack and heart failure have adverse implications for a patient’s prognosis, there are notable differences between the two conditions.
Heart Attack Prognosis:
- The prognosis of a heart attack is influenced by immediate complications, such as arrhythmias or cardiogenic shock, and the extent of myocardial damage.
- Prompt medical intervention, including reperfusion therapy, significantly improves short-term mortality rates.
- Survivors of a heart attack have an increased long-term risk of future cardiovascular events and mortality compared to the general population.
Heart Failure Prognosis:
- The prognosis of heart failure is influenced by the underlying cause, disease severity, response to treatment, and adherence to management strategies.
- Heart failure is associated with increased mortality rates, particularly in advanced or severe cases.
- Effective management strategies, including medications, device implantation, and lifestyle modifications, can improve symptoms, slow disease progression, and enhance quality of life.
Conclusion: Heart attack and heart failure have distinct prognostic implications for patients. While the immediate complications of a heart attack can be life-threatening, prompt medical intervention significantly improves short-term mortality rates. Survivors of a heart attack are at an increased long-term risk of future cardiovascular events and mortality. In contrast, heart failure is associated with increased mortality rates and reduced quality of life. Effective management strategies that slow disease progression, alleviate symptoms, and optimize cardiac function can positively impact the prognosis of heart failure. Understanding the differences in prognosis between heart attack and heart failure is crucial for healthcare providers in developing appropriate treatment plans and offering patient support.
| Aspect | Heart Attack | Heart Failure |
|---|---|---|
| Anatomy | Blockage of coronary artery leads to reduced blood flow to the heart muscle | Impaired pumping function or relaxation of the heart muscle |
| Symptoms | – Chest pain or discomfort (angina) – Shortness of breath – Sweating – Nausea or vomiting | – Fatigue – Shortness of breath – Swelling in legs, ankles, or abdomen – Reduced exercise tolerance |
| Diagnosis | – Electrocardiogram (ECG) – Blood tests (troponin levels) – Coronary angiography | – Echocardiogram – Electrocardiogram (ECG) – Blood tests (BNP levels) – Chest X-ray |
| Treatment | – Reperfusion therapy (PCI or thrombolytic therapy) – Medications (antiplatelets, beta-blockers, etc.) | – Medications (diuretics, ACE inhibitors, etc.) – Device implantation (ICD, CRT) – Lifestyle modifications |
| Prognosis | Increased short-term and long-term risk of cardiovascular events and mortality | Increased mortality rates and reduced quality of life |
Multiple Choice Practice Questions
Question 1: Which of the following conditions is characterized by a sudden blockage of blood flow to a coronary artery, leading to damage to the heart muscle?
A) Heart Attack B) Heart Failure C) Arrhythmia D) Atherosclerosis
Question 2: Which condition is often caused by weakened heart muscles unable to pump blood effectively, leading to inadequate circulation and fluid buildup in the lungs and other body tissues?
A) Heart Attack B) Heart Failure C) Aortic Stenosis D) Myocarditis
Question 3: What is the primary symptom of a heart attack?
A) Fatigue and weakness B) Shortness of breath and coughing C) Chest pain or discomfort D) Swelling in the ankles and legs
Question 4: Which diagnostic test is commonly used to detect heart attacks by assessing changes in cardiac enzymes and biomarkers?
A) Echocardiogram B) Electrocardiogram (ECG) C) Cardiac catheterization D) Blood pressure measurement
Question 5: In which condition does the heart’s pumping ability become compromised, leading to insufficient blood supply to the body’s organs and tissues?
A) Heart Attack B) Heart Failure C) Angina Pectoris D) Hypertension
Question 6: Which treatment option is a common intervention for a heart attack, involving the restoration of blood flow through the blocked coronary artery?
A) Beta-blockers B) Angioplasty and stent placement C) Diuretics D) Cardiac resynchronization therapy
Question 7: What anatomical event distinguishes heart attack from heart failure?
A) Blockage of a coronary artery B) Inadequate blood supply to the heart C) Weakening of heart muscle contraction D) Enlargement of the left ventricle
Question 8: Which condition is associated with chronic fatigue, fluid retention, and difficulty breathing, especially during physical activity?
A) Heart Attack B) Heart Failure C) Atrial Fibrillation D) Myocardial Infarction
Question 9: Which diagnostic tool assesses the heart’s structure, function, and blood flow through sound waves, helping to diagnose heart failure?
A) Cardiac catheterization B) Magnetic Resonance Imaging (MRI) C) Electrocardiogram (ECG) D) Echocardiogram
Question 10: What is a potential long-term consequence of repeated heart attacks on the heart’s structure and function?
A) Improved cardiac muscle strength B) Decreased blood pressure C) Increased cardiac output D) Reduced pumping ability and risk of heart failure
Answers and Explanations
Question 1: Which of the following conditions is characterized by a sudden blockage of blood flow to a coronary artery, leading to damage to the heart muscle?
Answer: A) Heart Attack
Explanation: A heart attack, also known as myocardial infarction, occurs when a coronary artery becomes blocked, usually due to a blood clot, resulting in damage to the heart muscle due to lack of blood flow and oxygen.
Question 2: Which condition is often caused by weakened heart muscles unable to pump blood effectively, leading to inadequate circulation and fluid buildup in the lungs and other body tissues?
Answer: B) Heart Failure
Explanation: Heart failure is a condition in which the heart’s pumping ability is compromised, resulting in inadequate circulation of blood and the accumulation of fluid in the lungs and other parts of the body.
Question 3: What is the primary symptom of a heart attack?
Answer: C) Chest pain or discomfort
Explanation: The primary symptom of a heart attack is chest pain or discomfort, often described as a heavy or squeezing sensation in the chest. It may radiate to the arms, neck, jaw, or back.
Question 4: Which diagnostic test is commonly used to detect heart attacks by assessing changes in cardiac enzymes and biomarkers?
Answer: B) Electrocardiogram (ECG)
Explanation: An electrocardiogram (ECG) is commonly used to detect heart attacks by recording the electrical activity of the heart. Changes in the ECG pattern can indicate damage to the heart muscle.
Question 5: In which condition does the heart’s pumping ability become compromised, leading to insufficient blood supply to the body’s organs and tissues?
Answer: B) Heart Failure
Explanation: In heart failure, the heart’s pumping ability is compromised, resulting in inadequate blood supply to the body’s organs and tissues, leading to symptoms such as fatigue and fluid retention.
Question 6: Which treatment option is a common intervention for a heart attack, involving the restoration of blood flow through the blocked coronary artery?
Answer: B) Angioplasty and stent placement
Explanation: Angioplasty involves inserting a balloon-tipped catheter to open a blocked coronary artery, and a stent is often placed to keep the artery open, restoring blood flow and preventing further damage.
Question 7: What anatomical event distinguishes heart attack from heart failure?
Answer: A) Blockage of a coronary artery
Explanation: A blockage of a coronary artery, usually by a blood clot, characterizes a heart attack. Heart failure involves the heart’s inability to pump blood effectively due to weakened muscles.
Question 8: Which condition is associated with chronic fatigue, fluid retention, and difficulty breathing, especially during physical activity?
Answer: B) Heart Failure
Explanation: Heart failure often leads to chronic fatigue, fluid retention (edema), and difficulty breathing, especially during physical exertion due to inadequate circulation.
Question 9: Which diagnostic tool assesses the heart’s structure, function, and blood flow through sound waves, helping to diagnose heart failure?
Answer: D) Echocardiogram
Explanation: An echocardiogram uses sound waves to create images of the heart’s structure, function, and blood flow. It is a valuable diagnostic tool for evaluating heart failure.
Question 10: What is a potential long-term consequence of repeated heart attacks on the heart’s structure and function?
Answer: D) Reduced pumping ability and risk of heart failure
Explanation: Repeated heart attacks can lead to significant damage to the heart muscle, resulting in reduced pumping ability and an increased risk of heart failure, where the heart struggles to meet the body’s needs.
Check out this popular article on the heart blood flow pathway steps!
Have a Great Day! 😀
Check out these popular articles 🙂
Circulatory System: Blood Flow Pathway Through the Heart
Ectoderm vs Endoderm vs Mesoderm
Circulatory System: Heart Structures and Functions
Ductus Arteriosus Vs Ductus Venosus Vs Foramen Ovale: Fetal Heart Circulation
Cardiac Arrhythmias: Definition, Types, Symptoms, and Prevention
Upper Vs Lower Respiratory System: Upper vs Lower Respiratory Tract Infections
Seven General Functions of the Respiratory System
Digestive System Anatomy: Diagram, Organs, Structures, and Functions
Kidney Embryology & Development: Easy Lesson
Psychology 101: Crowd Psychology and The Theory of Gustave Le Bon
Introduction to Evolution: Charles Darwin and Alfred Russel Wallace
Copyright © 2023 Moosmosis Organization: All Rights Reserved
All rights reserved. This essay first published on moosmosis.org or any portion thereof may not be reproduced or used in any manner whatsoever
without the express written permission of the publisher at moosmosis.org.

Please Like and Subscribe to our Email List at moosmosis.org, Facebook, Twitter, Youtube to support our open-access youth education initiatives! 🙂
Categories: anatomy, Biology, cell biology, education, health, medicine, stem, technology









Incredible medical articles!
LikeLiked by 1 person
Wonderfully written essay on heart attacks and heart failure!
LikeLiked by 1 person