Are you a medical student interested in pain medicine and pain management? Or, perhaps, want to learn more about the pharmacology or interventional procedures of pain medicine? Then, you’ve come to the right place to learn about the basics of pain management! In this succinct, easy-to-understand lesson, we learn about pain medicine, pain management for both acute and chronic pain, as well as pharmacology and interventional pain management. All on aboard!
Medical School: Pain Management on Acute and Chronic Pain
Pain can occur acutely or chronically, and adequate pain management is important for patients because it has been found to reduce risk of adverse outcomes, enhance quality of life, improve physical and psychological functionality, as well as shorten hospital stay. Adverse outcomes can include both circulatory and respiratory depression, nausea and vomiting, sedation, among many. If undertreated, patients can suffer thromboembolic complications, with increased stress, blood pressure, and the increased development of chronic pain. There are 3 main goals of pain therapy: including pain management offered around the clock, providing continuous pain relief, and assessing and reassessing patient for adequate pain relief.
3 main goals of pain therapy include 1) offering pain management around the clock, 2) providing continuous pain relief, and 3) assessing and reassessing for adequate pain relief!
Pain Management for Medical School: Acute Pain
There are two pillars of managing acute pain: 1) pharmacologic and 2) interventional. Pharmacologically, physicians can either alter nerve conduction with local anesthetics or modify transmission in the spinal column with opioids or antidepressants. One interventional technique is called the TAP (transverse abdominis plane) block that anesthetizes the peripheral nerves supplying the anterior abdominal wall (T6 to L1). For opioid analgesics like morphine, it is important to note the route of transmission, where oral of 300 is equivalent to parenteral 100, epidural of 10, and intrathecal of 1.
Always remember the dosage equivalents for opioid analgesics
Especially in NY State, healthcare providers monitor the use of opioids in patients. Patients can only get opioids from one MD, and often physicians check the ISTOP website to ensure patient is not getting opioids from another physician. For inpatient patients, a common pain management is patient-controlled analgesia or PCA. The patient has an IV where they can administer small doses of analgesic like opioids. PCA, however, is controlled and over dosage is prevented by the set limit of amount, number of boluses during a time period. What about ambulatory surgery? Compared to inpatient, ambulatory surgery patients do not use PCA and are often discharged within a few hours after surgery. Their pain is usually controlled with PO analgesics.
Inpatient Pain Management vs Ambulatory Surgery Pain Management?: PCA (inpatient) vs PO analgesics (ambulatory and discharge)
Pain Management for Medical School: Non-opioid Analgesics
Non-opioid analgesics are effective as well for treating patients in pain. Acetaminophen and NSAIDS such as aspirin, ibuprofen, ketorolac, COX-2 inhibitors, and Lidoderm are common non-opioids. NSAIDS are for mild to moderate relief but do have side effects including GI bleeding, nephrotoxicity, and inhibition of platelet aggregation which can potentially impact post-op bleeding. Ketorolac or Toradol is a potent analgesic and given parenterally including IV or IM; the typical dosage of ketorolac is 15-30 mg q6 hours with fewer side effects including minimal respiratory depression, no nausea/vomiting, and no pruritis. Cox-2 inhibitors include celecoxib (100-200 mg PO BID), rofecoxib, valdecoxib, or parecoxib.
NSAIDS: mild-to-moderate relief < Ketorolac or Toradol: moderate-enhanced relief
Pain Management for Medical School: Interventional Pain Management and Regional Nerve Block Anesthesia
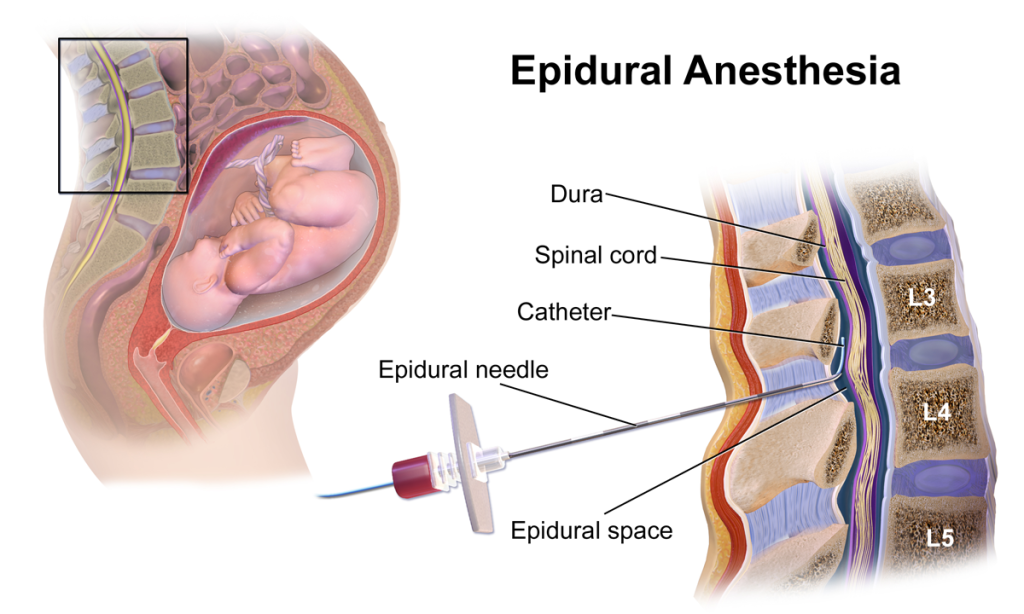
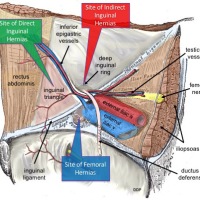
Interventional management includes 1) epidural analgesia, 2) spinal analgesia, and 3) peripheral nerve block. Epidural anesthesia can involve lumbar, thoracic, or caudal. Compared to general anesthesia, regional anesthesia has superior pain relief and fewer systemic side effects with lower incidence of DVT/PE and rapid recovery. However, there are absolute contraindications to be noted, including increased intracranial pressure, skin infection, coagulopathy.
During your inpatient clinical rotations or surgeries, you may see patients receiving epidural analgesia, which is commonly seen especially for mothers in labor and delivery! OBGYN ALERT! Remember, epidural analgesia for labor and delivery C-sections usually occur at L3-L4 or L4-L5.
Here is a diagram of epidural analgesia in action:
Regional anesthesia or nerve blocks are helpful for managing pain for patients in certain locations of their body, such as their back, lower legs, shoulders, etc. For example, before a patient goes for an orthopedic surgery to fix his or her broken bone, anesthesiologists or pain management interventionalists come in to perform a nerve block. They use an ultrasound to look at the anatomical structures underneath, finding the nerve and then use a needle to insert at the location and give regional anesthesia. This numbs the pain in that specific regional location and reduces systemic side effects.

Check out these popular articles 🙂
Circulatory System: Blood Flow Pathway Through the Heart
Ectoderm vs Endoderm vs Mesoderm
Circulatory System: Heart Structures and Functions
Ductus Arteriosus Vs Ductus Venosus Vs Foramen Ovale: Fetal Heart Circulation
Cardiac Arrhythmias: Definition, Types, Symptoms, and Prevention
Upper Vs Lower Respiratory System: Upper vs Lower Respiratory Tract Infections
Seven General Functions of the Respiratory System
Digestive System Anatomy: Diagram, Organs, Structures, and Functions
Kidney Embryology & Development: Easy Lesson
Autocrine vs Paracrine vs Endocrine: What are the Differences?
Their Eyes Were Watching God: Mule Symbol
Shoulder Abduction Muscles: Medical Anatomy and USMLE
Cell Membrane Dynamics: Flippase vs Floppase vs Scramblase
Cell Membrane Fluidity: Factors That Influence and Increase the Cell Membrane Fluidity
Psychology 101: Crowd Psychology and The Theory of Gustave Le Bon
Introduction to Evolution: Charles Darwin and Alfred Russel Wallace
An Overview of Shorthand: History and Types of Shorthand
Calculus: Two Important Theorems – The Squeeze Theorem and Intermediate Value Theorem
Copyright © 2023 Moosmosis Organization: All Rights Reserved
All rights reserved. This essay first published on moosmosis.org or any portion thereof may not be reproduced or used in any manner whatsoever
without the express written permission of the publisher at moosmosis.org.

Please Like, Share, and Subscribe to our Email List at moosmosis.org, Facebook, Twitter, Youtube to support our open-access youth education initiatives! 🙂
Categories: anatomy, Biology, cell biology, education, health, medicine, psychology, stem










This is such an important topic! Outstanding points and superb essay!!
LikeLiked by 2 people
Thank you so much Athena! Have a super day!
LikeLiked by 2 people
You’re welcome Moosmosis and you too!!
LikeLiked by 1 person
Excellent article on pain management!
LikeLiked by 2 people
Thank you so much K. Stevenson! Have an excellent day!
LikeLiked by 1 person
Very insightful! Thank you for shedding light on pain management, an essential part of many daily lives.
LikeLiked by 2 people
Thank you so much Dr. Keys! Happy to do so!
LikeLiked by 1 person
This is so helpful thanks!! I subscribed!
LikeLiked by 2 people
Thank you so much, Susan! Welcome to our community!
LikeLike
Fascinating!!
LikeLiked by 2 people
Thank you! Happy learning! 😀
LikeLiked by 1 person
Thank you so much!!
LikeLiked by 1 person